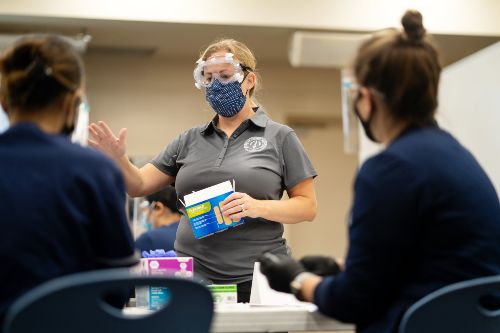
Those at the frontlines of the healthcare industry don’t just work in hospitals.
As the COVID pandemic has made clear, frontline professionals also include health navigators and coaches, nonprofit healthcare administrators, public health project managers and advocates, health data analysts, epidemiologists—and a long list of other experts seeking to build community health.

In fact, healthcare that’s focused on prevention, health maintenance and access to care and delivered in the community is among the fastest-growing sectors of the industry, including in the islands, said Chaminade School of Nursing and Health Professions Associate Dean Dr. Pamela Smith.
Smith said Chaminade is helping to meet that strong demand for community health with its unique Bachelor of Science in Community and Public Health, launched in Fall 2020. The innovative program has already attracted significant interest and is preparing graduates for a host of new opportunities.
“Our community really needs community health workers,” said Smith. “They are trusted in our communities, which means patient outcomes are better. Because of that, there’s a significant demand for graduates with this degree and they are very employable after graduation.”
Chaminade’s four-year Community and Public Health degree puts a strong emphasis on individualized instruction, hands-on learning, service to others in the community and mentorship. Students can choose from one of four specializations: Community Health Worker, Environmental and Health, Non-profit Administration and Data Analytics, all of which feature a strong foundation of knowledge.

Smith, who oversees the program, said the specializations were designed following in-depth conversations with community stakeholders and significant research into Hawaii’s healthcare needs. Each one gives students a host of potential career options or opportunities for further study.
“For example,” Smith said, “as a patient care manager, you would be looking at medical records, communicating with the patient, communicating with support agencies to improve health outcomes and access to care. Or in data analytics, perhaps you’d be studying information from pedometers to make conclusions about broader trends and to find potential solutions to boost patient health.”
“There are so many potential pathways to success,” Smith added.
The degree also prepares students to take the national Certified Health Education Specialist exam.
Participants in the Community and Public Health program complete foundational coursework in everything from human biology to science writing, and from bioethics to intercultural communication. Additional specialized study is offered in health disparities, the impact of environment on human health, organizational leadership and behavior and community-engaged computing and data analytics.
Going forward, Smith hopes to continue to expand the program as it attracts more students, especially by extending networking opportunities and offering students additional service-learning experiences.
“This program prepares students to work in the field of healthcare and public health outside of traditional patient care environments,” she said. “The simple truth is community and public health workers have the power to help people live healthier lives, reaching their fullest health potential.”